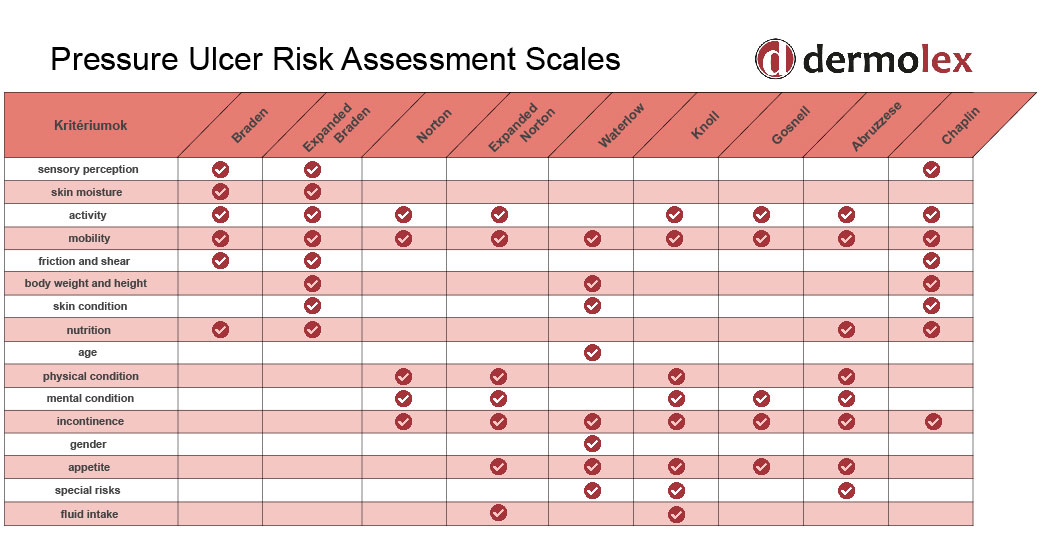
The Norton Scale and expanded Norton Scale are both used to predict the likelihood of developing a bedsore/decubitus, thus the scales can help to prevent it.
Decubitus is an immobilization syndrome. The statistics don’t look great regarding immobilized patients: both hospitalized patients and the ones who are treated at home are likely to suffer from this ailment. The chance of developing a bedsore is 14%. Having decubitus is painful and the treatment process can be long and costly because it requires special skills and knowledge to help the patient heal. Also, at least two nurses are needed to treat the patient because changing someone’s position is difficult. It also slows the patient care process.
It’s important to know the rules of how to prevent and treat decubitus and what are the symptoms because home-treated people can also develop this malady.
Decubitus is an immobilization syndrome
Decubitus ulcers are open skin wounds that develop because of pressure. Patients who are laying all day long can easily develop decubitus: prolonged pressure, shear, or friction damages the skin causing death to cells and tissues.
There is a subtype of bedsores: in this case, the deeper tissues are already dead but a thin layer of skin still covers the wound.
Preventing decubitus with dermolex
Prevention is a key factor to save the patient from unnecessary pain and discomfort. The symptoms emerge slowly and if attention isn’t paid, the condition can worsen rapidly. It is important to take care of the patient’s skin by changing their position in the bed several times a day and using a gel that heals your skin.
Dermolex gel is recommended for normal and sensitive skin. It should be used on the areas of the body which are most likely to be affected:
- The back or sides of the head
- Shoulder blades
- Spine
- Elbows
- Lower back and tailbone
- Hips
- Buttocks
- The backs of the knees
- Ankles
- Heels
Learn more about prevention and the dermolex gel.
Norton scale
The chances of having decubitus are different for each individual. The Norton scale is a method that gathers the relevant information to determine the chances.
Risk factors examined with the Norton scale:
- Physical condition
- Mental condition
- Activity
- Mobility
- Incontinence
Doctors assign a value to the various factors on a scale from 1 to 4.
| Physical condition | Good (4) | Fair (3) | Poor (2) | Very bad (1) |
| Mental condition | Alert (4) | Apathetic (3) | Confused (2) | Stuporous (1) |
| Activity | Ambulant (4) | Walks with help (3) | Chairbound (2) | Bedfast (1) |
| Mobility | Full (4) | Slightly impaired (3) | Very limited (2) | Immobile (1) |
| Incontinence | None (4) | Occasional (3) | Usually urinary (2) | Urinary and fecal (1) |
Incontinence means the lack of voluntary control over urination or defecation.
In the casual Norton scale, you can ‘earn’ points from 5 to 20. The lower the score the more likely the pressure ulcer is going to develop.
Medium risk category: points between 14-12
High-risk category: points lower than 12.
In the case of medium risk, increased attention is needed to notice if something is not right with the affected areas mentioned above.
In the case of high risk, actions are needed immediately.
Expanded Norton scale
The expanded Norton scale has 9 factors to examine.
- Physical condition
- Mental condition
- Activity
- Mobility
- Incontinence
- Age
- Skin condition
- Additional diseases
- Cooperation
Points range from 9-36 points.
- Above 25 points, there is a low risk.
- Medium risk between 25-20 points
- High risk between 20-13 points
- Very high risk below 13 points
| Cooperation | Full (4) | Less (3) | Partly (2) | None (1) |
| Age | <10 (4) | <30 (3) | <60 (2) | 60+ (1) |
| Skin condition | Good (4) | Scaly, dry (3) | Moist (2) | Wounds (1) |
| Additional diseases | None (4) | Undermine of resistance, diabetes (3) | Multiple sclerosis, adiposis (2) | Artery occlusion (1) |
The Norton scale seems easy to examine yourself, but it’s only effective if a doctor or nurse who is competent to determine the real risks and conditions use it. Even if the patient is treated at home, an expert’s assistance is advised.
Braden scale
The Braden scale also shows the risk of developing decubitus, but with different factors. The Braden scale is the most popular method which takes into account six factors:
- Sensory perception: completely limited, very limited, slightly limited, no impairment
- Skin moisture: constantly moist, very moist, occasionally moist, rarely moist
- Activity: Bedfast, chairfast, walks occasionally, walks frequently
- Mobility: completely immobile, very limited, slightly limited, no limitation
- Nutrition: very poor, probably inadequate, adequate, excellent
- Friction and shear: problem, potential problem, no apparent problem
Read more about the Braden scale.
Decubitus recovery time
Healing from a decubitus ulcer can take weeks or even months. It depends on the patient’s age, additional diseases, and other above-mentioned risk factors. Decubitus also has more stages: healing time from stage 2 is between 1-6 weeks, but recovering from the 4th stage takes several months (and there is a chance of never properly recovering).
Summary of bedsores and how to prevent them
The treatment of decubitus is not easy. It has a painful and long recovery time. In the case of young people, it mostly develops after paralytic diseases or accidents that cause immobility. For elderly people, it can appear after only a few days spent in the hospital so it is advisable to prevent it: starting from the first day in the hospital.
Recovery time varies after reaching different stages of decubitus. The Norton scale helps to identify the risks of developing pressure ulcers.
When preventing decubitus, the most important thing is frequent rotation (several times a day) of the patient. Change the patient’s position and use dermatologically tested regenerating, circulatory enhancing skin protective gel, like dermolex.