Moisture associated skin damage is a general term used to describe skin damage caused by prolonged exposure to moisture. Moisture can come from a variety of sources including perspiration, saliva, mucous, and wound drainage. However, the main culprit is faecal and/or urinary incontinence. Prolonged exposure to moisture makes the skin more penetrable and decreases its effectiveness as a barrier.
The symptoms of MASD include inflammation of the affected area and skin breakdown, which can appear as if the skin is decaying. Friction, in addition to the prolonged exposure to moisture, can cause the skin to tear, thereby allowing pathogens to enter the wound. These injuries can lead to secondary infections of the impacted skin.
People with limited mobility, whether recovering from an accident/surgery or residents of long term care facilities, are at an increased risk of moisture associated dermatitis, as are people suffering from obesity and diabetes mellitus. Up to half of long-term-care residents are reported to have the inability to control their urinary function and up to 2/3 are reported to be unable to control their faecal function. Aging skin loses its elasticity and becomes thinner and drier which makes the elderly population more susceptible to moisture associated skin damage.
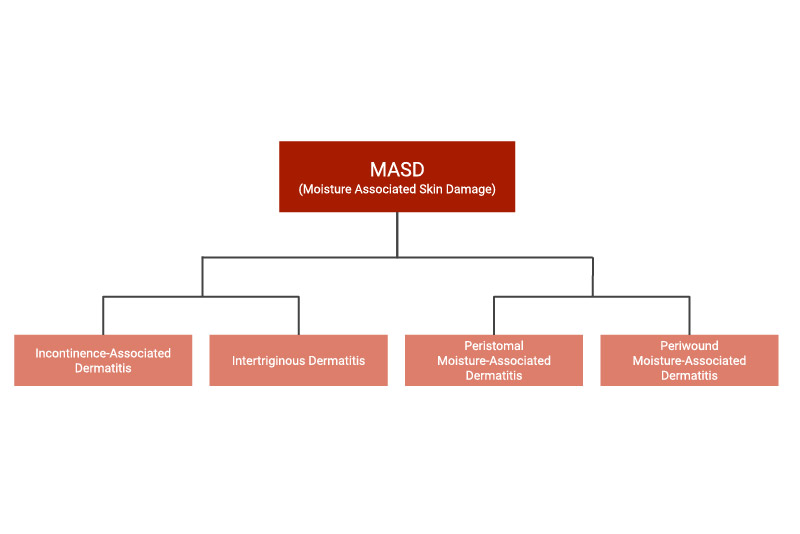
Types of Moisture-Associated Skin Damage
Incontinence-Associated Dermatitis (IAD)
Most commonly referred to as ’diaper rash,’ IAD occurs when skin is exposed to urine, stool, or liquid stool for a prolonged period of time. Incontinence Associated Dermatitis can develop in the area between the anus and the scrotum or vulva (including the labial folds), the groin, the buttocks, the groove between the buttocks, and the inner and rear portions of the thighs.
Intertriginous Dermatitis (ITD)
Also called intertrigo, ITD is caused when perspiration collects in the folds of the skin and that skin rubs together. The areas of the body where this commonly occurs are: the groin, armpits, underneath the breasts, and the stomach, although any area of the body where there is a skin fold is an at risk area. This type of moisture associated skin damage most often affects those who are suffering from obesity, diabetes mellitus, and/or are bedridden.
Peristomal Moisture-Associated Dermatitis
This type of MASD specifically affects those living with a temporary or permanent ostomy. It occurs when discharge from the ostomy comes into prolonged contact with the skin and causes inflammation and erosion of the skin. Poorly fitting containment devices are the main culprit, so it is of utmost importance that a secure fit of the device is established and maintained throughout its use.
Periwound Moisture-Associated Dermatitis
When skin is exposed to exudate for a prolonged period of time, periwound moisture associated dermatitis can occur. Exudate is a liquid produced by the body that oozes at the site of inflammation or a lesion. It contains proteolytic enzymes that can damage the outer layer of skin. Wound exudate is a natural part of the healing process, but prolonged exposure to this type of moisture can cause maceration. Macerated skin can lead to longer healing times and increase the risk of infection.
Prevention and Treatment of Moisture-Associated Skin Damage
In order to prevent MASD, the 3 main principles are cleanse, protect, and restore:
- Cleanse the skin daily using a mild product with a pH factor close to that of normal skin and gently pat dry. No rinse cleansers can help avoid extra friction.
- Frequently change incontinence pads/liners/briefs.
- Immediately change soiled undergarments.
- Always cleanse the skin immediately following an episode of incontinence.
- Apply a barrier product in order to protect the skin from moisture.
- Use an emollient to help keep skin supple and moisturized, but consult with a doctor to avoid over hydration.
To treat moisture associated dermatitis:
- Reduce pressure on the affected area in order to increase dryness and reduce the risk of friction.
- Identify the source of moisture.
- Determine the type of urinary and/or faecal incontinence. Is it the result of tube feeding or a bacterium (such as Clostridium difficile)?
- Track any patterns. What time of day does the incontinence occur?
- Eliminate any foods that may induce incontinence (caffeine, carbonated beverages, spicy foods, acidic foods such as citrus fruits and juices, etc.).
- Include foods that are rich in fibre and contain active yogurt cultures (lactobacillus)
- Take medication if necessary.
- Seek surgical treatment if necessary.